The Great Medical Data Extraction: Who Pays for the Future of Health?
Why hasn't digital health transformed the clinic yet? We break down the crippling friction points: the AI-EHR collision, the telehealth hangover, and the coming war over your personal wearable data
TECNOLOGYDIGITAL HEALTH
1/12/2026

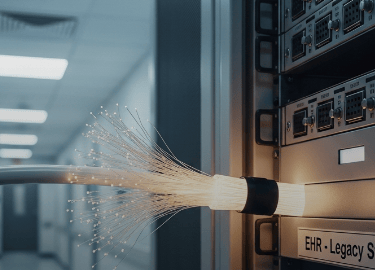
The promise of seamless, personalized medicine often ends with a data export button trapped in a secure portal you forgot the password to. Silicon Valley sold us a revolution—a world where the Apple Watch prevents the heart attack and AI flags the cancer years early. The sensors and algorithms are here; the connectivity is a disaster. The current digital health pulse isn't one of rapid innovation, but of brutal integration. The excitement surrounding new devices and diagnostic breakthroughs is tempered by the grim reality that medicine remains a business rooted in decades-old infrastructure and bureaucratic friction. We are currently watching billion-dollar health-tech firms slam up against the unyielding wall of the Electronic Health Record (EHR). This is where the digital future of health lives or dies: not in the lab, but in the operational trenches of the American hospital.
1The Bot in the Room: AI Diagnostics Hit the EHR Wall
AI excels at pattern recognition—sifting through millions of CT scans, pathology slides, or genomic sequences faster than any human team. But the real bottleneck isn't the algorithm’s intelligence; it’s the 15-year-old EHR system it has to talk to. Hospitals spend staggering sums licensing cutting-edge AI tools, only to find the data pipes are clogged. An AI designed to spot early signs of diabetic retinopathy needs timely, high-quality images and patient history, but retrieving that data often requires complex, manual workarounds because the systems were never designed for two-way automation. Clinicians don't want another siloed dashboard they must log into; they need the diagnostic insight woven directly into their existing workflow—a workflow already optimized for exhaustion and liability avoidance. Furthermore, the friction is heavily regulatory: the FDA approves the algorithm’s performance under controlled conditions, but hospitals must vouch for its safety and efficacy within their own messy, unique environments. This gap between academic breakthrough and scalable, bedside care is the integration chasm that is swallowing massive investments.
2Virtual Care Fragmentation and the Quest for Quality
Telehealth exploded in 2020 out of sheer necessity, establishing a proof-of-concept that virtual care was viable. Now, the market is correcting, focusing on return on investment (ROI) rather than mere convenience. We are moving past simple video calls as the metric of success. Investors are demanding proof that virtual care saves money and demonstrably improves long-term outcomes for chronic conditions, not just offers easier scheduling. This scrutiny has led to a highly specialized and fragmented landscape. The market is now a dizzying array of condition-specific vertical companies: digital diabetes management platforms, remote mental health services, and hypertension apps, each optimized for a narrow slice of care. While specialization drives powerful results within that niche, it risks creating a highly fragmented patient experience. A single patient might interact with five different health apps, none of which communicate effectively with their primary care provider, the hospital system, or each other. The next phase requires brutal consolidation and deep interoperability, proving that a virtual interaction isn't just cheaper, but truly equivalent or superior to the holistic care provided in person.
3The Body as a Data Source: When Wellness Meets Wallet
Millions of people now wear devices that generate a constant, granular stream of physiological data: sleep scores, heart rate variability, glucose levels. This information is medically valuable—a true picture of daily health behavior—yet it lives almost exclusively in proprietary silos managed by tech companies like Google, Apple, and Oura, not healthcare providers. The central friction point is governance and trust. When a device detects an anomaly suggesting AFib or severe sleep apnea, who owns the liability if the user ignores the warning, or if the alert is a false positive? And crucially, who profits when this aggregated population data—scrubbed of personal identifiers, perhaps, but still highly valuable—is sold to pharmaceutical researchers, insurance actuaries, or consumer goods developers? We are fast approaching a flashpoint where users realize their steps, stress levels, and nightly oxygen saturation are not just vanity metrics, but currency. They are beginning to demand clearer utility, stronger control, and explicit consent mechanisms that move beyond the simplistic 'I agree' scroll button. The battle for who owns your daily biometrics is the silent legal fight defining the next decade of personal health.
The Bottom Line
The digital health revolution isn't failing; it’s simply relocating the fight from the academic lab to the legislative floor and the billing department. This means that better, more targeted diagnostics and preventative insights are undeniably coming. However, they will likely arrive first for those who can afford specialized corporate wellness programs or premium, cash-pay subscription models. The current struggles over integration, regulatory clarity, and data ownership are delaying the benefits of technology for the mass market. True equity in digital health requires demanding that the software built to analyze our deepest biological data must also be capable of communicating flawlessly with the lowest-funded community clinics. Until the infrastructure is fixed, the future of health will remain trapped in a series of expensive, disconnected beta tests.
#DIGITAL HEALTH
#AI IN MEDICINE
#TELEHEALTH ROI
#BIOMETRIC DATA GOVERNANCE
#EHR INTEROPERABILITY
Copyright @HealthTechnos 2025. All Rights Reserved
Subscribe Now
Join us for health updates!
