The Data Flood: Are Health Metrics Helping or Harming Us?


Introduction
The Data Flood has become a defining feature of modern health tracking, shaping how people understand their bodies every day.
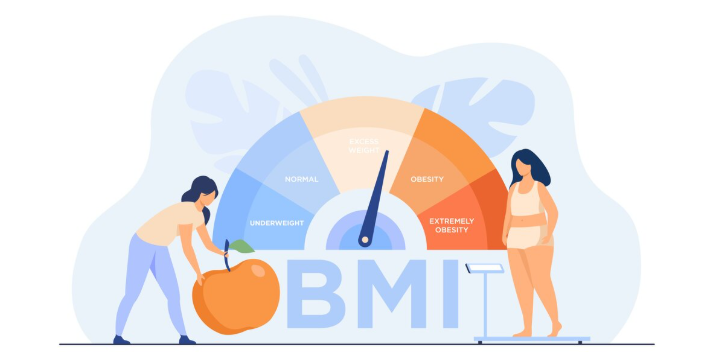
From steps and sleep to heart rate and calories, numbers now guide many personal health decisions.
Wearable technology and apps promise clarity and control. However, constant measurement can also confuse and overwhelm.
Therefore, it is important to ask whether all this information truly supports well-being or quietly creates new problems.
Understanding The Data Flood in Modern Health
The Data Flood refers to the massive amount of health data generated by digital tools and wearables.
These insights aim to empower users with real-time feedback about daily habits.
Moreover, access to detailed metrics can motivate healthier routines.
For example, tracking sleep patterns may encourage better rest.
Yet, without context, raw numbers often lack meaningful guidance.
How Health Metrics Can Help Us
Health data works best when paired with self-awareness. Metrics can reveal patterns, but true wellness comes from understanding context, emotions, and physical signals together, not from numbers alone.
Health tracking offers clear advantages when used wisely.
Metrics can highlight trends that people might otherwise miss.
In addition, digital dashboards simplify complex health information.
Smartwatches and fitness gadgets collect data continuously, helping users notice progress and stay accountable to their goals.
When The Data Flood Becomes Overwhelming
The Data Flood can also create stress instead of reassurance.
Many users feel pressure to meet daily targets, even when their bodies need rest.
However, constant alerts and comparisons may lead to anxiety.
Therefore, people sometimes prioritize numbers over intuition, ignoring natural physical signals.
Psychological Effects of Constant Health Tracking


Living inside The Data Flood can shift focus from overall wellness to perfectionism.
A single bad metric may ruin an otherwise healthy day.
Moreover, overanalyzing data often increases self-judgment.
As a result, mental fatigue grows while motivation declines, especially when goals feel unreachable.
Finding Balance in The Data Flood
Managing The Data Flood starts with selective attention.
Not every metric deserves equal importance, and not every fluctuation signals a problem.
Helpful ways to regain balance include:
- Tracking only essential metrics
- Reviewing trends weekly instead of hourly
- Listening to physical and emotional cues
- Taking occasional breaks from tracking
In addition, limiting reliance on screens helps reconnect with natural body awareness beyond numbers.
Are We Measuring Health or Chasing Numbers?
The rise of The Data Flood raises an important question about intention.
Health data should inform decisions, not dictate self-worth.
Moreover, technology works best as a guide, not a judge.
When users control their tools, instead of the reverse, data becomes supportive rather than stressful.
The Bottom Line
“Data should inform health, not define it. When numbers guide curiosity instead of control, technology becomes a partner in wellness rather than a source of stress.”
Ultimately, The Data Flood is neither entirely helpful nor harmful.
Its impact depends on how thoughtfully it is used.
By combining data awareness with self-compassion, people can turn health metrics into allies instead of sources of pressure.
For Nutritional Health related articles Click here